Prescription Drug Benefit
Prescription Drug Benefit
West Virginia Senior Advantage (HMO I-SNP) provides Medicare Part D prescription drug coverage through its partner, ElixirOptions.
ElixirOptions is a healthcare and pharmacy benefit management (PBM) company headquartered in North Canton, Ohio.
We have over 1500 employees supporting a rapidly growing membership base of over 21 million members, creating savings for them as well as thousands of plan sponsors. Rite Aid’s acquisition of Elixir in 2015 brings together two national healthcare companies that give consumers more pharmacy options, and plan sponsors improved manufacturer relationships and analytic capabilities.
For your convenience, there is a complete list of all covered drugs in the plan (a comprehensive formulary). Our Online Formulary lists the Part D drugs covered by West Virginia Senior Advantage. Our formulary is designed to cover the drugs most needed to treat the special needs of our members.
If the drug you are taking is not on the list of covered drugs, read your Prescription Drug Transition Policy and Evidence of Coverage to find out what you can do. This includes instructions for both new and current members.
West Virginia Senior Advantage Plan Rating (Part D only). The Star Ratings Program is based off of CMS’ Quality Strategy of optimizing health outcomes by improving quality and transforming the health care system. View our Star Rating.
For Prescribers & Pharmacies
West Virginia Senior Advantage provides Medicare Part D prescription drug coverage through our partner Elixir.
Elixir is a full-service pharmacy benefit management company committed to lowering drug costs, improving health, and providing superior customer service in a manner that instills trust and confidence.
For Prescribers:
- Elixir Pharmacy Helpdesk
- Phone number: 1-833-665-5423
- TTY phone number: 711
- Refer to the Prescription Drug Benefit page for formulary, prior authorization criteria, and step therapy criteria
For Pharmacies:
- Elixir Pharmacy Helpdesk
- Phone number: 1-833-665-5423
- TTY phone number: 711
- Refer to the Prescription Drug Benefit page for formulary, prior authorization criteria, and step therapy criteria
Member Part D Prescription Drug Benefits
Below is a brief summary of benefits. For a complete list of benefits and other resources, please review your Evidence of Coverage.
How much do I pay?
For Part B drugs such as chemotherapy drugs: 20% of the cost Other Part B drugs: 20% of the cost
Initial Coverage
After you pay your yearly deductible, you pay 25% of the cost for all drugs covered by this plan until your total yearly drug costs reach $4,430. Total yearly drug costs are the total drug costs paid by both you and our Part D plan.
You may get your drugs at network retail pharmacies.
If you reside in a long-term care facility, you pay the same as at a retail pharmacy. You may get drugs from an out-of-network pharmacy at the same cost as an in-network pharmacy
Coverage Gap
Most Medicare drug plans have a coverage gap (also called the “donut hole”). This means that there’s a temporary change in what you will pay for your drugs. The coverage gap begins after the total yearly drug cost (including what our plan has paid and what you have paid) reaches $4,430.
After you enter the coverage gap, you will pay no more than 25% coinsurance for generic drugs or 25% coinsurance for brand name drugs, for any drug tier during the coverage gap.
Catastrophic Coverage
After your yearly out-of-pocket drug costs (including drugs purchased through your retail pharmacy and through mail order) reach $7,550, you pay the greater of:
- 5% of the co insurance, or
- $4.15 copay for generic (including brand drugs treated as generic) and a $10.35 copayment for all other drugs.
If you have questions or want to request additional information , please call Member Services at 1-833-665-5423. TTY users should call 711. Live representatives are available 24 hours a day, 7 days a week.
How to Request a Coverage Determination
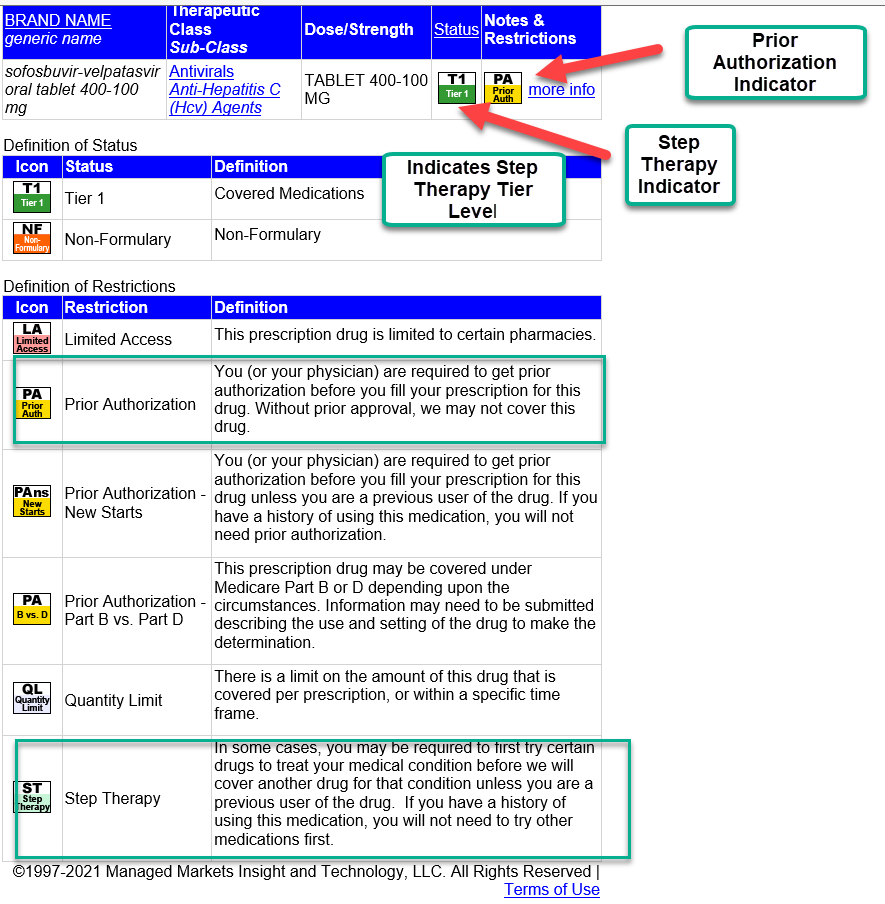
Prescription Utilization Management Step Therapy and Prior Authorization Criteria
West Virginia Senior Advantage Health Plan members can find Part D prescription Step Therapy and Prior Authorization Criteria by clicking on the Online Drug List under the Prescription Drug Benefit topics or at the Online Drug List Link below: